Periodontitis is a common yet often overlooked oral health issue. Whether you’ve heard of it before or not, understanding periodontitis is crucial for maintaining a healthy smile. So, let’s dive right in and explore this condition, its stages, prevention strategies, treatment options, and more!
What is periodontitis?
Periodontitis, also known as gum disease, is a chronic bacterial infection that affects the gums and surrounding structures supporting the teeth. It is a progressive condition that, if left untreated, can lead to tooth loss and other serious oral health problems.
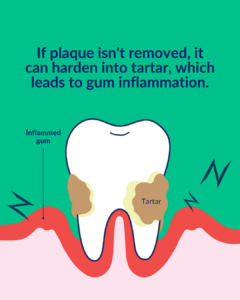
When plaque, a sticky film containing bacteria, builds up on teeth and gums, it can cause inflammation. This initial stage is called gingivitis. If gingivitis is not addressed, it can progress into periodontitis, where the infection spreads below the gumline and affects the supporting tissues and bone.
What are the causes of periodontal diseases?
Understanding the causes of periodontal disease is essential in preventing and managing this oral health condition. Let’s explore some of the primary factors that contribute to the development of periodontal disease:
- Plaque buildup:

Plaque, a sticky film composed of bacteria, food particles, and saliva, constantly forms on the teeth. If not effectively removed through proper oral hygiene practices, plaque can harden into tartar (calculus), which can only be removed by a dental professional. Tartar provides a breeding ground for bacteria, leading to gum inflammation and periodontal disease. - Poor oral hygiene: Inadequate oral hygiene practices, such as infrequent or improper brushing and flossing, can contribute to the development of periodontal disease. Insufficient plaque removal allows bacteria to thrive and lead to gum inflammation.
- Tobacco use: Smoking or chewing tobacco is a significant risk factor for periodontal disease. Tobacco use weakens the immune system, reduces blood flow to the gums, and impairs the healing process, making it more difficult to combat and control gum infections.
- Hormonal changes: Hormonal fluctuations, such as those experienced during puberty, pregnancy, and menopause, can make gums more sensitive and susceptible to inflammation. Hormonal changes can also alter the body’s response to bacteria, increasing the risk of periodontal disease.
- Systemic diseases: Certain systemic conditions, such as diabetes, cardiovascular disease, and autoimmune disorders, can increase the risk and severity of periodontal disease. This may be due to the impact these diseases have on the body’s immune response and overall oral health.
It’s important to note that while these factors increase the likelihood of developing periodontal disease, they do not guarantee its occurrence. Maintaining good oral hygiene practices, adopting a healthy lifestyle, and seeking regular dental care can significantly reduce the risk of periodontal disease and promote optimal gum health.
What are the stages of periodontal disease?
Periodontal disease progresses through several stages, each with its own characteristics and implications for oral health. Here are the main stages of periodontal disease:
- Gingivitis: This is the earliest stage of gum disease and is characterised by red, swollen, and bleeding gums. Fortunately, at this stage, the damage can be reversed with proper oral hygiene and professional dental cleanings.
- Early periodontitis: As the disease progresses, the supporting bone and connective tissues start to break down. Pockets form between the gums and teeth, trapping food particles and bacteria. At this stage, professional intervention is necessary to halt the progression and prevent further damage.
- Moderate periodontitis: The bone and connective tissues continue to deteriorate, and the pockets become deeper. Teeth may become loose or shift in position, affecting bite and overall oral function.
- Advanced periodontitis: This is the most severe stage of gum disease, where significant bone loss occurs. Teeth may become very loose or even fall out. In some cases, extensive dental treatments, such as extractions or dental implants, are required.
What is the difference between gingivitis and periodontitis?
As mentioned above, Gingivitis and periodontitis are both forms of gum disease, but they differ in terms of severity and the extent of damage caused. Gingivitis is the milder form, affecting only the gums and characterised by inflammation, redness, and bleeding. With proper oral care and professional dental cleanings, gingivitis can be reversed.
On the other hand, periodontitis is a more advanced stage of gum disease where the infection has spread below the gumline, affecting the bone and supporting tissues. It is marked by the formation of periodontal pockets, gum recession, tooth mobility, and potential tooth loss. Unlike gingivitis, periodontitis cannot be fully reversed but can be managed and stabilised with appropriate treatment.
What are some symptoms of periodontal diseases?
Periodontal disease can present with a variety of symptoms, which can vary depending on the stage and severity of the condition. Here are some common symptoms to be aware of:
- Gum inflammation: Swollen, red, and tender gums are early signs of gum disease. Healthy gums should appear pink and firm, so any noticeable changes in their appearance or texture may indicate an underlying issue.
- Bleeding gums: Bleeding during brushing, flossing, or even spontaneously is a common symptom of gum disease. Healthy gums should not bleed, so if you consistently notice blood when cleaning your teeth, it’s important to seek dental attention.
- Gum recession: As periodontal disease progresses, the gums may recede or pull away from the teeth. This can lead to the exposure of tooth roots, causing sensitivity to hot or cold temperatures.
- Bad breath: Persistent bad breath, also known as halitosis, can be a sign of gum disease. The odour is often caused by the bacteria and toxins produced by the infection.
- Deep pockets: In advanced stages of periodontal disease, deep spaces or pockets can form between the gums and teeth. These pockets trap food particles and bacteria, leading to further inflammation and damage to the supporting structures.
- Loose or shifting teeth: As periodontal disease progresses, the bone and connective tissues that hold teeth in place can be compromised. This can result in teeth feeling loose, shifting position, or changes in the bite.
- Pus between teeth and gums: In severe cases of periodontitis, pockets of pus may develop, causing a foul taste in the mouth and discharge when pressure is applied to the gums.
- Changes in bite or difficulty chewing: If teeth are shifting or becoming loose due to periodontal disease, it can affect the alignment of the bite and make chewing uncomfortable or challenging.
It’s important to remember that periodontal disease can be present even without experiencing obvious symptoms. Regular dental check-ups and professional cleanings are therefore vital for early detection and intervention. If you notice any of these symptoms or have concerns about your gum health, it’s recommended to consult with a dental professional who can assess your condition and recommend appropriate treatment.
How to treat periodontitis?
Treating periodontitis involves a combination of professional dental care and self-care practices. The specific treatment plan may vary depending on the severity of the disease. Here are some common treatment options:
- Scaling and root planing: This deep cleaning procedure is performed by a dental professional to remove plaque and tartar from below the gumline. It also involves smoothing the tooth roots to prevent further plaque buildup.
- Periodontal surgery: In advanced cases, periodontal surgery may be necessary to access and clean the deep pockets and to repair or regenerate damaged tissues.
- Antibiotics: In some cases, your dentist may prescribe antibiotics to control bacterial infection and reduce inflammation.
- Ongoing maintenance: After the initial treatment, regular dental visits for professional cleanings and check-ups are crucial to monitor your oral health and prevent disease progression.
Your dentist will create a personalised treatment plan based on your specific needs. It’s important to follow their instructions and attend all recommended follow-up appointments to achieve the best possible outcomes. Find out more about gum treatment at WeSmile Dental.
How to prevent periodontitis?
Preventing periodontitis starts with a proactive approach to oral hygiene and regular visits to your dentist. Here are some essential steps you can take to reduce your risk:
- Brushing: Brush your teeth thoroughly at least twice a day using a soft-bristle toothbrush and fluoride toothpaste. Pay special attention to the gumline and use gentle, circular motions to clean effectively without causing irritation.
- Flossing: Don’t forget to floss daily! This helps remove plaque and debris from between the teeth and along the gumline, where a toothbrush can’t reach effectively.
- Healthy diet: Opt for a balanced diet rich in vitamins and minerals, as this can strengthen your immune system and promote gum health. Limit sugary and acidic foods and drinks, as they can contribute to tooth decay and gum disease.
- Avoid tobacco: Smoking and chewing tobacco significantly increase the risk of developing periodontitis. Quitting tobacco can greatly improve your oral and overall health.
- Regular dental visits: Schedule regular dental check-ups and professional cleanings. Your dentist can detect and treat any early signs of gum disease before they progress.
By following these preventive measures, you can significantly reduce the likelihood of developing periodontitis and maintain a healthy smile.
Other FAQs about periodontitis and treatment
Is it possible to cure periodontitis at home?
While it’s essential to practice good oral hygiene at home, periodontitis cannot be fully cured through home remedies alone. The disease requires professional intervention to effectively manage and prevent further damage. However, you can support your treatment by following a diligent home care routine and maintaining regular dental visits.
At home, make sure to brush your teeth thoroughly at least twice a day and floss daily to remove plaque and debris. Additionally, using an antimicrobial mouthwash as recommended by your dentist can help reduce bacteria and prevent plaque buildup.
Remember, even if your symptoms improve or disappear, it’s crucial to continue with your prescribed treatment plan to prevent a recurrence of the disease.
Can antibiotics cure periodontal disease?
While antibiotics can play a role in the treatment of periodontal disease, it’s important to note that they are not a cure on their own. Antibiotics are often prescribed as an adjunctive therapy to control the bacterial infection and reduce inflammation.
In cases where the infection is severe or has spread, antibiotics may be used in conjunction with scaling and root planing or periodontal surgery. However, it’s crucial to remember that antibiotics should only be taken as prescribed by your dentist, and completing the full course of medication is essential to maximise their effectiveness.
Can periodontal disease be reversed?
While periodontitis cannot be fully reversed, it can be managed and stabilised with appropriate treatment and ongoing care. With early intervention and diligent oral hygiene practices, it is possible to prevent further damage and maintain oral health.
Treatment aims to control infection, reduce inflammation, and halt the progression of the disease. Regular dental visits, professional cleanings, and a dedicated home care routine are essential to successfully managing periodontal disease in the long term.
How to get rid of bad breath from periodontal disease?
Bad breath, or halitosis, is a common symptom of periodontal disease. The odour is typically caused by the bacterial infection and the accumulation of plaque and debris in the periodontal pockets. While addressing the underlying gum disease is essential, there are some additional steps you can take to improve bad breath:
- Maintain proper oral hygiene: Brush your teeth at least twice a day, floss daily, and use an antimicrobial mouthwash to reduce bacteria and freshen breath.
- Clean your tongue: Use a tongue scraper or your toothbrush to gently clean the surface of your tongue. Bacteria can accumulate on the tongue and contribute to bad breath.
- Stay hydrated: Drink plenty of water throughout the day to keep your mouth moist and reduce the risk of dry mouth, which can worsen bad breath.
- Avoid strong-smelling foods: Certain foods like garlic and onions can contribute to bad breath. Limiting their consumption can help improve your breath.
If bad breath persists despite these measures, it’s important to consult your dentist for a comprehensive evaluation and appropriate treatment.
What are the brushing techniques for periodontal disease?
Proper brushing techniques are crucial for maintaining gum health, especially for individuals with periodontal disease. Here’s a step-by-step guide to effective brushing:
- Choose the right toothbrush: Opt for a soft-bristle toothbrush that can effectively clean your teeth and gums without causing irritation. Electric toothbrushes with rotating or oscillating heads can also be beneficial.
- Position the brush: Hold your toothbrush at a 45-degree angle towards the gumline.
- Brush gently: Use short, circular or vibratory motions to clean the outer and inner surfaces of your teeth. Pay extra attention to the gumline, where plaque tends to accumulate.
- Don’t forget the chewing surfaces: Brush the chewing surfaces of your teeth using back-and-forth motions.
- Brush your tongue: Gently brush your tongue to remove bacteria and freshen your breath.
- Rinse thoroughly: After brushing, rinse your mouth thoroughly with water or an antimicrobial mouthwash.
Remember to brush at least twice a day for a minimum of two minutes each time. It’s also a good idea to replace your toothbrush or brush head every three to four months or sooner if the bristles become frayed.
Is periodontal disease contagious?
Periodontal disease is not contagious in the same way as a cold or flu. However, the bacteria responsible for gum disease can be transmitted between individuals through saliva, especially through activities such as sharing utensils, kissing, or intimate contact.
While the transmission of these bacteria alone does not guarantee the development of gum disease, it can increase the risk for susceptible individuals. Therefore, it’s crucial for individuals with periodontal disease to maintain good oral hygiene and avoid activities that could potentially transmit the bacteria to others.
Prevent periodontal disease with quality dental care
In conclusion, periodontitis is a common yet manageable oral health condition. By understanding its stages, implementing preventive measures, seeking professional treatment, and maintaining good oral hygiene practices, you can effectively manage periodontal disease and enjoy a healthy smile for years to come.
Need more guidance and advice on what to do next to treat your gums? Learn more about our gum treatment options or book an appointment with us using the form below!



